Long-term effects of hypoparathyroidism:
Complications of the disease
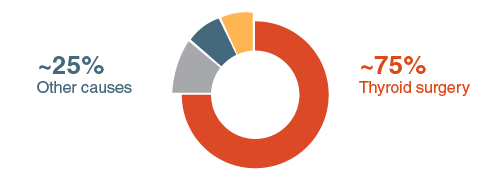
Hypoparathyroidism (hypopara) is a rare endocrine disease, which causes inadequate levels of parathyroid hormone (PTH) to be secreted by the parathyroid glands in the neck. This results in a mineral imbalance in the body expressed by a low concentration of calcium (hypocalcaemia) and a high concentration of phosphate (hyperphosphatemia) in the blood. For some patients, hypopara will be a chronic life-long condition that requires careful management throughout their lives. The most common cause of hypopara is as a result of thyroidectomy or neck surgery which has caused damage to the parathyroid glands. However, hypopara can also be genetic, caused by autoimmune disorders, or be idiopathic (no known cause) which can impact patients from childhood. The symptoms of hypopara may include but are not limited to tingling and twitching of muscles; muscle spasms or cramps; confusion and memory loss; weak and brittle nails; bone weakness; and brain fog and fatigue. For some patients, these symptoms can often be controlled with the use of calcium and vitamin D supplements (conventional treatment), but for a number of people this treatment will not be sufficient. When hypopara is not managed effectively, the comorbidities and complications can be significant, particularly to the brain, kidneys and heart, as well as impact patient quality of life (QoL).
Complications associated with inadequate
management of hypopara
Some of the most common symptoms of hypopara are caused by hypocalcaemia and the effect it has on the nervous system, including physical symptoms such as tingling, twitching and muscle spasms; and cognitive symptoms, such as brain fog and memory loss. Calcium has an important role in the signalling of nerves throughout the body and in the brain. A lack of calcium can lead to a disruption in this signalling. This can often lead to serious complications, such as seizures. Seizures are particularly common for idiopathic patients who are affected from childhood and throughout their lives, with ~60-70% experiencing seizures as a symptom. Anti-epileptic drugs are usually used for the treatment of seizures.
Hypopara can usually be managed with calcium and vitamin D supplements, which reduce the symptoms associated with hypocalcaemia. When supplementation does not adequately manage hypopara, is used over a long period or at the wrong dose, hypercalcaemia (high levels of blood calcium) may occur. Hypercalcaemia can sometimes lead to too much calcium being deposited around the body (known as extraskeletal calcifications). Calcifications are rare, but very serious, so doctors and endocrinologists must monitor blood and urinary calcium, phosphate, and calcium phosphate product* closely to minimise the risk. Calcifications can occur in the kidney, leading to kidney stones; in the eyes, causing cataracts; or in the brain, causing seizures. Complications associated with hypercalcaemia may be influenced by age, how long they have had hypopara and how long they have been having treatment. Physicians may choose to reduce calcium dosage if necessary to minimise the risks of hypercalcaemia. Closely monitoring calcium-phosphate product also enables physicians to assess the risk of renal complications, including chronic kidney disease and kidney failure. Elevated levels of calcium-phosphate product have been associated with an increased risk of renal diseases. A high calcium-phosphate product may also increase calcifications over time. Other risk factors for risk of renal disease include having hypopara for more than 12 years and having four or more hypercalcaemic episodes. Physicians may regularly monitor for renal complications, but patients can also help by keeping their physician informed about hypercalcaemic episodes or any changes in their symptoms.
The Impact of Hypopara on Quality of Life (QoL)
Another complication of hypopara is the long-term impact the disorder has on patient QoL. The symptoms of hypopara are often difficult to manage and can have an effect on patients both physically and mentally. Patients may find day-to-day activities more difficult because their symptoms reduce their physical ability. Whereas, brain fog or fatigue can also make cognitive tasks more challenging. The symptoms of hypopara can have a wider on impact patients careers, relationships, physical ability and mental health, which can cause an overall reduction in their QoL. Symptoms of hypopara may have a direct influence on these factors, such as brain fog and fatigue impacting their ability to focus at work, or tetany and muscle spasms reducing physical ability. Some patients also report an impact on their mental health, with depression and anxiety, emotional sensitivity and isolation as common symptoms. Patients may consider seeking support from family, friends or a patient group. Physicians may advise speaking to a mental health professional to help with mental symptoms or refer patients to a physiotherapist for exercises to improve muscle.