DIAGNOSIS
Hypoparathyroidism (hypopara), through the various symptoms it causes, can disrupt everyday life by affecting:
- Movement (muscular spasms, twitching, bone pain)
- Cognition (brain fog, seizures, memory loss)
- Emotional well-being (anxiety, depression)
- Work (reduced dexterity, lapses in concentration, fatigue)
- Personal relationships (feeling isolated, low self-esteem, poor self-image)
Because hypopara is so rare, and the symptoms differ from person to person, they may not be recognised as being caused by hypopara.
A simple blood test can indicate hypopara. The diagnosis can then be confirmed by other evaluations such as a physical assessment, looking at medical history, and a urine test. Hypopara is defined as blood calcium levels below the normal range (hypocalcaemia), with abnormally low or completely absent levels of parathyroid hormone. The normal concentration of calcium in the blood is 2.10–2.60 mmol/L.
If you have been diagnosed with hypopara, it can help to let any medical professional who may be treating you know, so they can get the correct treatment for you quickly.
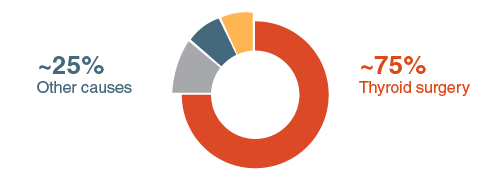
The main cause of hypopara is removal of or accidental damage to the parathyroid glands during neck surgery.
The doctor may ask you about your surgical history, and perform a physical examination.You may have your medical records reviewed for other conditions, such as kidney or gastrointestinal illnesses, as well as any medications and supplements you are currently taking.
If your hypopara does not appear to have an obvious surgical cause, genetic testing may be considered, particularly if you are of a young age or have a family history of hypopara. Genetic testing can be used to identify a genetic mutation that may be causing the disease, and can help to inform family planning.
Your doctor may test you for the physical signs and symptoms of hypopara
One of the major physical signs of hypopara is muscular excitability, where your muscles are agitated and may twitch or contract easily. The doctor will perform a number of different physical assessments of your muscles and nerves. These may include:
– Testing your reflexes.
– Tapping the side of your face to see if it elicits a twitching response, to test your muscles for over-excitability.
– Restricting the blood flow in your arm to see if it causes your hand and finger muscles to contract or twitch.
– Testing your muscles for weakness by asking you to perform simple tasks.
– Asking you if you are experiencing tingling, numbness, or hot and cold sensations in the tips of your fingers, toes, or other parts of your body.
– Your doctor may listen to your heart to check for signs of an irregular heartbeat, known as an arrhythmia, as well as listening to your lungs to check for wheezing, difficulty breathing, and throat tightness.
– Some hypopara patients may have calcium deposits in their eyes or joints. Your doctor may examine the eyes for cataracts and the joints for restricted range of motion.
The major biochemical sign of hypopara is having lower than normal levels of calcium (hypocalcaemia) combined with absent or deficient levels of parathyroid hormone (PTH) in the blood.The doctor may take a blood sample and assess the calcium and PTH levels. This should be carried out on at least two separate occasions at least two weeks apart. Your calcium and PTH levels will naturally fluctuate for 6 months following neck surgery. Therefore, you can only be diagnosed with chronic hypopara if you are still experiencing symptoms 6 months after your operation.
Taking calcium supplements to help treat hypopara can cause higher than normal amounts of calcium being excreted in the urine. If this is untreated, it may lead to complications such as calcium deposits in the kidneys and kidney stones. Therefore, calcium levels in the urine need to be closely monitored, and if they are too high, your doctor may adjust your medication to minimise the risk of side-effects.
Physical examination following diagnosis looks at the skeleton, which is commonly affected by the disease. In some cases, the doctor may take an X-ray of the skull, to identify if there are any calcium deposits in the brain. The doctor may also perform an ultrasound or CAT scan of the kidney in order to identify any kidney stones or renal calcifications. Finally, the doctor may perform a test, known as dual energy X-ray absorptiometry, to determine the density of the bones.
The doctor may be interested in other biochemical that look at kidney function.